When most people hear the word cartilage, it brings to mind joints in the hip, knee, shoulder, wrist, or finger. Rarely do you hear about costal cartilage.
So, What Exactly Is Costal Cartilage?
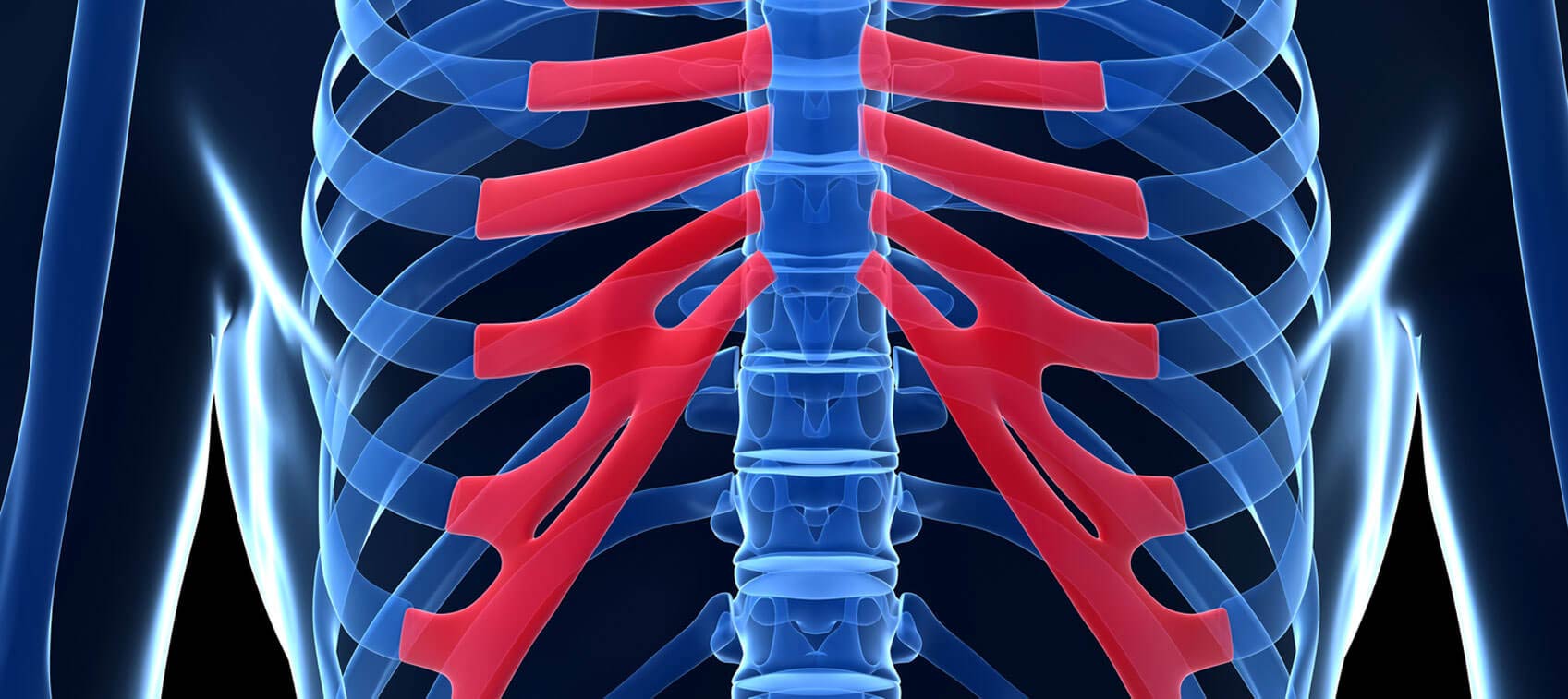
Costal cartilage is the fibrous cartilage that attaches your ribs to your sternum (breastbone). Specifically, costal cartilage directly connects the first through the seventh ribs to the sternum.
The eighth, ninth, and tenth ribs are referred to as “false ribs” since they don’t attach directly to the sternum, but rather are secured to the seventh rib by costal cartilage. While the remaining two lower, short ribs are attached to the spine, they aren’t secured to the front of the chest. That’s why they’re called “floating ribs.”
While costal cartilage firmly attaches the ribs to the sternum, it still allows for a degree of flexibility. This is important because the chest and thoracic structure need to be rigid enough to protect the heart, lungs, and other internal organs—yet elastic enough to allow for some movement and expansion of the chest cavity. This elasticity lets the lungs fully expand during breathing and enables us to twist our upper body.
Costal Cartilage Damage and Pain
Costal cartilage is part of the continuous “link” between the sternum, spine, collarbone, shoulders, and arms. Any blunt-force trauma to the chest, shoulders, sides, or back can be transferred to the costal cartilage, resulting in tears, ruptures, or inflammation. This can happen with athletic injuries, falls, or other accidents.
Costal cartilage pain can also result from something as simple as sleeping in an odd position, twisting, or lifting. These are particularly common with age, since cartilage becomes less flexible.
The area can be very painful to touch, and most people will notice the discomfort during twisting or when changing positions in bed. It can also feel like a sharp, stabbing pain when taking a deep breath. Women may find the aches more severe when wearing a bra. Movements like lifting or pushing, sitting for long periods of time, sneezing, or blowing your nose may exacerbate the pain.
Costal cartilage pain can be very sharp in the region of the sternum, but it can also feel like a stabbing pain in the upper back between the shoulder blades. Sometimes it is even mistaken for a heart attack.
Treatment for Costal Cartilage Pain
The standard treatment for costochondritis (inflammation of costal cartilage) is to prescribe over-the-counter anti-inflammatory medicine like ibuprofen, with the hopes that the costal cartilage pain and inflammation will subside in a week or two.
If that doesn’t fix the issue, it’s often followed up with corticosteroid injections, which rarely provide a long-term solution. In some chronic cases, surgery is even recommended.
Unfortunately, all of these “treatments” are merely addressing symptoms, not the underlying causes of the costal cartilage pain—and the patient continues to suffer. Treatment really needs to focus on fixing two main causes: subluxation (misalignment) and hypothyroidism.
Misalignment
Oftentimes, physicians overlook the fact that there’s an actual joint where the ribs meet the sternum. Although there’s not a ton of movement here, it does move slightly when you breathe and twist your upper torso.
Early in life there's even a synovial membrane in these joints that produces a lubricating synovial fluid. Around middle age, the joint surfaces start to roughen; by old age, the joint cavity has pretty much closed.
Just like other joints in the body, the bones that form them can become misaligned. The misalignment can occur after some kind of accident or trauma (open heart surgery is just one example), or as mentioned earlier, sleeping in an odd position, twisting, or lifting. This is one very common cause of costal cartilage pain or costochondritis.
In these cases, a chiropractor can really help. A specific chiropractic adjustment to either the rib head at the spinal vertebra or to the rib at the costal cartilage/sternum joint will often provide quick and permanent relief.
Hypothyroidism
Hypothyroidism is another cause of costal cartilage pain, and it tends to affect women more than men. The discomfort will often occur at more than one rib/sternum junction joint, but especially between the second and third ribs. There are numerous associated reflex points in this area.
Thyroid problems and costal cartilage pain may seem like an unusual connection, but throughout history, health practitioners from many different healing disciplines noted that very specific areas of tenderness almost always co-existed with underlying organ dysfunction or pathology. Some of the areas correlate with acupuncture points and circuits that supply “energy” to the organs. Other areas correspond to the sympathetic fibers of the autonomic nervous system that are known to run along skin pathways. And some reflex points appear in locations where lymph tissue and nerve endings meet and become painful when there is a blockage of lymph flow in the area.
Different healing disciplines refer to them with different names. Osteopaths call them Chapman reflex points; chiropractors call them neurolymphatic points; and neurologists call them viscerosomatic points.
Correcting hypothyroidism will often alleviate this costal cartilage pain rather quickly. Two natural products I recommend for an underactive thyroid are the glandular Thytrophin PMG from Standard Process Laboratories, and the iodine supplement Iosol from TPCS Distributors. It's not unusual to see an immediate 50–75% reduction in pain after simply taking a few drops of Iosol.
Costal Cartilage Pain Is Curable
If you have costal cartilage pain, rest assured it is almost always a curable problem. It may be a matter of correcting thyroid dysfunction, or fixing misalignment and then refraining from certain activities until the supporting ligaments and tendons have had time to heal. As is the case with most health conditions, the key is making the proper diagnosis of the underlying problem, and not merely treating the symptoms.


