One of the frustrating aspects about getting older is the loss of being “bullet proof” when it comes to health. Most of us were fortunate enough as youngsters to not have to worry about the health consequences of our actions. That sure changes with age.
Cuts and wounds are no longer something to brag about and show our peers; they become a potential disability. Aches and pains seem to pop up for no reason, and injuries take longer to heal.
Much of our ability to recover from practically any health problem depends on the state and burden we place on our aging and overworked immune systems. Over and over we hear about the need to boost our immune system through diet, supplements, and exercise. What we rarely hear about, however, are steps we can take to lessen the burden on our immune system. And for the most part, people aren’t taking those necessary steps. This is evident from the high degree of chronic inflammation we see throughout our entire population.
Acute Inflammation vs. Chronic Inflammation
Inflammation (or the lack thereof) is one indicator of how efficiently and precisely our immune system is functioning. There are two categories of inflammation: acute and chronic.
Acute inflammation is the body’s healthy response to injury and infection. It consists of several parts: pain, heat, redness, and swelling. Following an injury or infection, the pain alerts us to the fact and keeps us from overusing the area and causing more injury. Redness comes from the increased temperature and circulation directed to the area, which brings along immune cells to fight infection and begin the repair process. Swelling “walls off” the area to keep infection or damage from spreading.
Acute inflammation, while sometimes uncomfortable, is a necessary part of the healing process. But chronic inflammation is a totally different matter.
Chronic inflammation starts off as acute, but the elimination of the pathogen or irritant never takes place. The repair process also never takes place. This can occur for several reasons. The body might not have the right raw materials to repair the problem; the onslaught of pathogens doesn’t stop; we keep feeding the body foods that cause irritation (for instance, too many pro-inflammatory omega-6 oils in relation to anti-inflammatory omega-3 oils); or the immune system begins to attack healthy tissue, as it does in many autoimmune diseases.
With chronic inflammation, the immune response never shuts off. The constant production of immune cells is not only draining to the body, but when tissues are under constant attack, it results in permanent damage. Healthy tissues are being subjected to a constant barrage of “friendly fire” from a perpetual war occurring within the body. Defense always takes precedence over repair. When your immune system is overwhelmed defending against pathogens, for example, the repair of damaged areas gets overlooked.
Inflammation Contributes to Countless Diseases
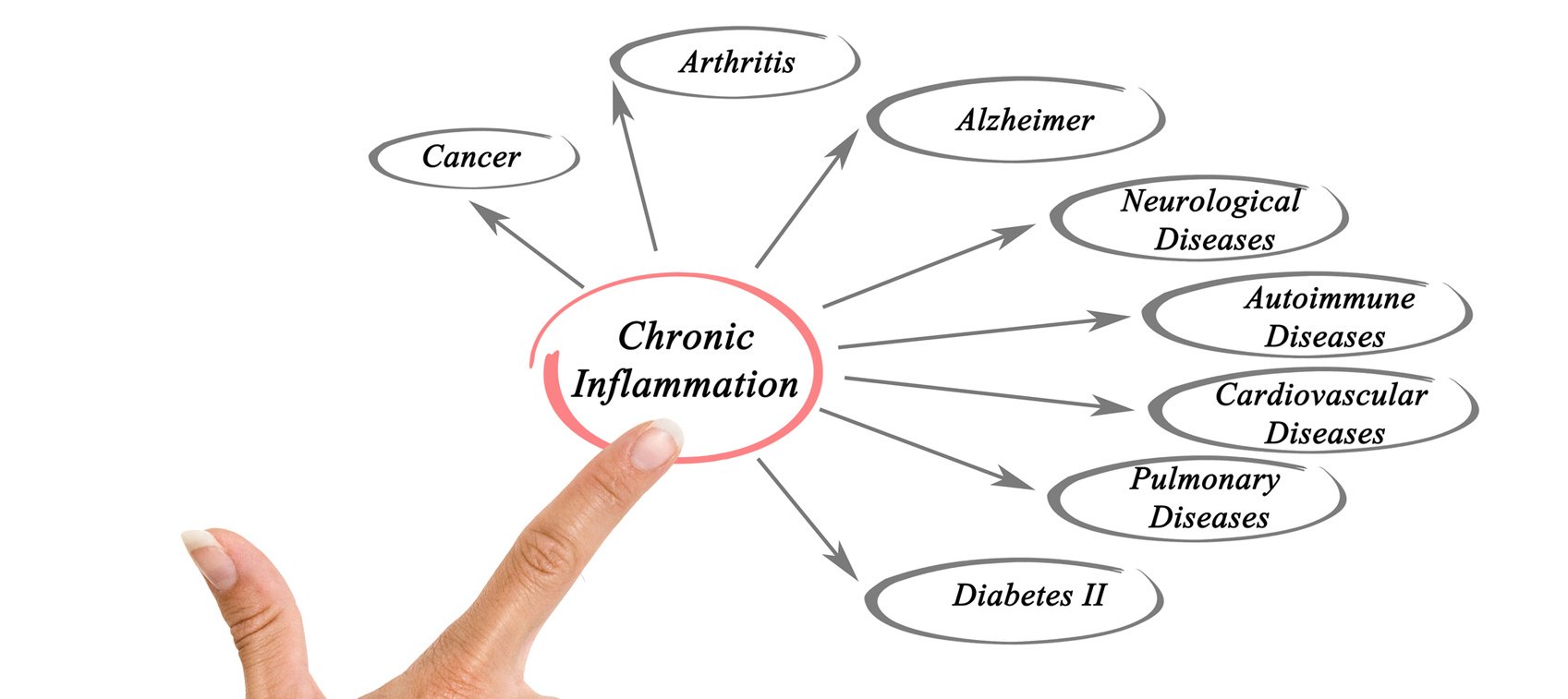
When you look at the most common diseases in our society, it’s glaringly obvious that chronic inflammation is rampant. Some of the diseases that chronic inflammation has been directly linked to include:
- Heart disease
- Stroke
- Arthritis
- Nerve degeneration
- Diabetes
- Metabolic syndrome
- Sarcopenia
- Kidney and lung destruction
- Autoimmune diseases
- High blood pressure
- Sleep apnea
- Inflammatory bowel disease
- Asthma
- Fibromyalgia
- Chronic fatigue syndrome
As a well-known and established contributing factor to disease, chronic inflammation has been documented in hundreds, if not thousands, of research studies. Conventional medicine and the pharmaceutical industry continue to capitalize on these findings.
Pharmaceutical companies produce inflammation blockers and anti-inflammatory drugs, and they are sold over the counter and prescribed by doctors by the millions. These drugs include everything from simple aspirin and over-the-counter NSAIDs to more sophisticated drugs that block nerve receptors in the body. The focus isn’t to reduce the actual cause of the inflammation, but instead to block its effects.
For the most part, these medications block the ongoing repair process, which, in turn, reduces the swelling and pain. But this blocking process just creates a vicious cycle of increased inflammation that requires even more immune suppression. It’s like having a gas fire burning in the body but rather than shutting off the fuel, they just keep spraying water on it. It just keeps burning.
How do you know if you have a problem with chronic inflammation? If you have any of the chronic diseases I mentioned earlier, or if you’re taking medication to treat any of those problems, you most likely have chronic inflammation.
And thanks to a solid body of research, we know what’s feeding a lot of these fires. Here are a few of the most common sources.
Inflammation Cause #1: Belly Fat
Fat cells used to be thought of as just a storage place for energy. New research in just the last decade has shown that the functions of fat cells are far more complex than we ever thought, and their functions vary depending on where they are located in the body. Abdominal fat cells are different from other fat cells in the body. Visceral (belly) fat plays a large role in insulin resistance, the stepping stone to diabetes and dementia.
Fat cells produce numerous hormones and chemical messengers that trigger inflammation throughout the body. (Men with waistlines that measure 40 inches or more, or women with waistlines that measure 35 inches or more, likely experience chronic inflammation as a result of that visceral fat—even if their body weight is normal.)
Fat cells also produce a hormone called leptin. In the simplest terms, leptin tells the brain to stop eating. (It also influences the thyroid gland and the adrenals.)
As you produce more fat cells, they produce more leptin to let the brain know that everything is okay, the body is full, and you need to stop eating.
When researchers discovered leptin, they thought they had found the answer to obesity. But when leptin was given to overweight individuals, it didn’t help, and that’s when we learned about “leptin resistance.” The fats cells produce more and more leptin but it never gets to the brain.
Leptin resistance is directly linked to insulin resistance. As you recall, insulin resistance results from consuming too many carbohydrates, or sugars. One of insulin’s primary jobs is to get cells to “open up” and allow glucose to enter. Over a period of time, a high-carbohydrate diet continues to flood the system with insulin, and cells can become resistant to the effects of insulin. When this happens, glucose (or blood sugar) isn’t moved into muscle cells where it can be utilized as energy.
To supply needed energy, the body releases stored fats, in the form of triglycerides, into the bloodstream to be used for energy, and blood sugar levels rise (i.e. type 2 diabetes).
It just so happens that high blood triglyceride levels also block leptin from reaching the brain.
Without leptin, there is no signal to the brain that the body needs to stop eating. Instead the brain thinks that the body is starving and actually increases the sensation of hunger.
High-carbohydrate diets create a vicious cycle of blood sugar–handling difficulties, increased appetite, fat accumulation, and greater levels of inflammation in the body. It’s no wonder that losing excess body fat will normalize blood sugar levels, eliminate type 2 diabetes, reduce inflammation, and reverse many of the related health problems I listed earlier.
Eliminate Belly Fat
To get rid of excess fat cells, you need to cut the simple carbohydrates out of your diet. Cutting out carbohydrates lowers triglyceride levels and helps allow leptin to reach the brain so it can tell your body to stop eating.
In the beginning, it’s not easy to cut carbohydrates out of the diet and, to be honest, it’s almost impossible to permanently strip excess fat from the body without some form of regular exercise.
Keep in mind that the body fat causing the most problems is the visceral fat. Unfortunately, in men, visceral fat is typically the first fat to accumulate and the last fat to be shed. In females, the last fat to go is in the thighs and buttocks. This is why you can’t selectively lose belly fat just by doing sit-ups or other abdominal exercises.
In addition to removing simple carbohydrates from your diet, take supplements such as conjugated linoleic acid (CLA), creatine, green tea extract, pinolenic acid, saffron extract (Satiereal), and whey protein, all of which help to reduce appetite or promote lean muscle development.
Bauhinia—a Leptin Regulator
Another natural plant extract appears to work on leptin’s ability to more effectively influence the hypothalamus, the part of the brain that acts as the body’s appetite center. This flowering tree, called the Brazilian Orchid tree, can be found in the Amazon. Its proper name is Bauhinia forficate (pronounced “bah-heen-yah”), and it’s also commonly known as Pata de Vaca (“paw of cow”).”
Traditionally, native populations used bauhinia to control their sweet tooth. As such, it has been referred to as “vegetable insulin.”
Not only does it control blood sugar levels, but it also possesses antibacterial and antifungal properties. Based on these characteristics, it has been used as a “blood cleanser.”
Dozens of studies dating all the way back to the 1920s and 1930s document the effective uses of bauhinia. Like many natural therapies, though, there were no financial motives or incentives to fund large scale studies on a non-patentable product. Except among the indigenous populations, there has been very little use of this amazing plant.
The majority of studies on bauhinia have demonstrated that it exhibits significant anti-diabetic activity. It’s not surprising that it would also lower cholesterol and triglycerides, act as a diuretic, and protect kidney function.
And although it might not be my first choice for venomous snake or scorpion bites (unless I was in the jungle without other options), research has shown it can be an effective treatment for those, too.
Although I learned about and witnessed the use of bauhinia 10 years ago in both Quito, Ecuador and various places in Brazil, only recently have I been able to find a US source for the herb. And what really reignited my interest in bauhinia was its link to leptin. It provides us with a new, effective method to help overcome leptin resistance and accelerate fat loss.
One four-week study compared the weight loss effects of a bauhinia extract to a placebo on a group of 31 overweight patients. The extract was given half an hour prior to each meal. At the end of the four weeks, the average weight loss in the treated group was 4.66 pounds, and waistline measurements decreased by over 1½ inches. The placebo group gained an average of ½ pound and ¼ inch in the waistline.
The study was extended for an additional four weeks, and the average weight loss among those taking the bauhinia was 12 pounds. In addition, waistlines decreased by three inches and hip measurements dropped almost two inches. It was interesting that, in this particular study, every individual taking the bauhinia extract lost weight.
Amazon Discovery sells a kilo of the bulk powder, which will last over five months. Click here for more information.
In South America, where the plant is used to treat diabetes, a cup of tea made by seeping the plant’s leaves can be taken three times daily (one cup following each meal). Reportedly 2 grams of the powdered extract can be substituted for a cup of the tea. Since it will lower blood sugar levels, those with diabetes should check with their doctor before using it, as blood sugars will need to be monitored.
Inflammation Source #2: Your Mouth
Our oral cavity is another very common source of chronic inflammation.
Offhand I can’t think of a single person who has spent more of his life studying and documenting the link between infections in the oral cavity and systemic diseases than Dr. Weston Price. His work on focal infections, endodontics, and nutrition continues with the Weston A. Price Foundation and the Price-Pottenger Nutrition Foundation, both of which are treasure troves of solid nutritional advice and guidelines.
The connection between periodontal disease and cardiovascular disease has been well documented. For years, people have been warned that periodontal disease and/or chronic gum infections increase the risk of developing heart disease. For some reason, many people don’t take these warnings too seriously. I think one reason is because the dental profession doesn’t stress this fact. It may also be that most people find it a stretch to understand how something happening in the mouth could cause heart or vascular problems.
Newer research, however, has definitively shown the presence of periodontal pathogens in atherosclerotic plaques. In other words, the bacteria and other pathogens that are causing your gums to bleed and stay infected move into the bloodstream, and trigger clogging in the arteries.
Another recent study compared various bacteria in the oral cavity and gut to those found in arterial plaque. For the most part, the pathogens in arterial plaque were more closely linked to those found in the mouth.
Transient bacteremia (or the entry into and movement of bacteria thorough the bloodstream) happens to everyone. This makes sense when you consider the rich blood supply in the mouth and how thin and fragile the skin around the gum is. This area is also subject to a lot of mechanical irritation from chewing, brushing, flossing, and dental procedures.
Under ideal conditions, the situation is controlled rather quickly by the immune system. But even then, some of the more persistent bacteria evade the immune system and reach the bloodstream. The problem is obviously worse in people who have bleeding gums and/or periodontal disease. Bleeding from periodontal disease provides pathogenic bacteria direct entry into the bloodstream.
The bottom line is, chronic periodontal disease equates to a chronic infection in the body. This, in turn, is one more reason that cardiovascular disease is the number-one cause of death in this country.
Cut Out Sugar, Control Harmful Oral Bacteria
Along with minimizing the amount of pathogenic bacteria that enter the bloodstream via the mouth, it is also wise to reduce the number of harmful bacteria in the mouth. This can be done a couple of ways.
Reducing sugar intake is the first step. Streptococcus mutans is the bacterium that causes dental caries (cavities). This bacterium forms the biofilm, plaque, or gooey, sticky, mucus-like substance that allows microorganisms to attach to the teeth and gum surfaces. These biofilms are very tough and protect the bacteria from destruction. Biofilms make these bacteria 1,000 times more tolerant of antibiotics. This is one of the primary reasons antibiotics haven’t been that effective in treating dental caries and tooth destruction.
Sucrose (sugar) is the only compound that S. mutans can use to make this biofilm. Also, sucrose changes the electrical charge and pH of the biofilm, which results in demineralization of tooth enamel and underlying dentin. Studies have repeatedly shown that you can reduce the number of S. mutans by decreasing your sugar intake.
When you introduce sugar into your mouth, the pH drops dramatically, making your mouth more acidic. An acidic environment starts the demineralization of the teeth and increases the activity of S. mutans. It is one of the only species of bacteria in the mouth that thrives under acidic conditions. The metabolism of most species slows when things become acidic. The metabolism of S. mutans actually improves. It creates even more acid, making the area more favorable for further bacteria growth. As a result, S. mutans quickly becomes the dominant bacterium.
I’ve written many times that sugar kills. We continue to learn that it does so in many different ways. Our ever-growing addiction to sugar has caused many of the systemic health problems we suffer from today.
Without sugar in the diet, S. mutans wouldn’t be a problem. Historical studies have demonstrated this to be the case. Weston Price showed the detrimental effects of introducing sugar into primitive societies. More recent studies have confirmed these findings. The changes have been documented in Inuit families, Norwegian children, and others, where sugar consumption was almost nil but increased due to changing circumstances.
Most of the bacterial species that inhabit us exhibit a symbiotic relationship that has evolved over time. For example, we feed and house species of bacteria in our colon and, in return, they manufacturer vitamin K or essential fatty acids that we need to survive. At one time, S. mutans probably didn’t cause any trouble and even helped prevent the colonization of harmful bacteria species. The widespread use of sugar changed the relationship.
Sugar has become such a huge part of our lives that most people will never be convinced that they need to remove it from their diets. And of course it has become almost impossible now to totally eliminate it. But the research is there. It is directly linked to the number-one disease responsible for more deaths than any other.
Most people (doctors included) don’t realize that S. mutans is the most prevalent bacterial species found in the artery cell walls of patients who undergo cardiovascular surgeries. And an infection by S. mutans is a leading cause of endocarditis or inflammation of heart valves.
Oral Probiotics Also Control Harmful Bacteria
Using an oral probiotic is another fundamental step you can take to reduce the number of pathogenic bacteria that reside in your oral cavity. It’s not just important as we grow older and are trying to take a load off our immune system. The problems associated with oral bacteria start early in life.
S. mutans is virtually undetectable in infants until around the age of two. However, babies delivered via Caesarean section have detectable levels a year earlier. Babies who pass through the vaginal canal have the benefit of being inoculated with bacteria naturally found in the birth canal. C-section babies don’t.
S. mutans is eventually transmitted to children primarily from their mothers and secondarily from exposure and contact to others. If the mother suffers from periodontal disease, the child is already placed at a disadvantage when it comes to developing dental caries and even heart disease, multiple sclerosis, and diabetes. (This is because dental disease and the associated bacteria have been suggestively linked to diabetes, high blood pressure, and multiple sclerosis later in life.)
That’s why I think oral probiotics are important for everyone.
The composition of oral probiotics is different from intestinal probiotics. The strains and balance of bacteria are totally different. But the goal is the same—trying to naturally promote the beneficial species of bacteria and establishing an environment that inhibits the growth of pathogenic bacteria.
“Oil Pulling” Improves Oral Bacterial Balance
Another largely forgotten technique to clean the oral cavity of toxins and pathogenic bacteria is called oil pulling.
I first learned about oil pulling when studying the ancient system of healing called Ayurvedic medicine that originated in India thousands of years ago.
The technique is very simple, although a little time consuming. But it does work, and it works well.
There are a lot of claims made regarding the benefits of oil pulling, which is nothing more that swishing a tablespoon of oil around in your mouth for up to 15 minutes before spitting it out. Personally, I can’t attest to the effectiveness of many of the claims (curing diabetes and cancer, pulling toxins from the blood, etc.), but it does balance the bacterial flora in the mouth and can significantly improve periodontal health.
Studies from India (where oil pulling originated and is still practiced) show that after 24 hours, 48 hours, one week, and two weeks, there were significant reductions in S. mutans counts in those who practiced oil pulling for 10 minutes each day before brushing.
It would probably be a good practice, but for most people, I’m not sure oil pulling is necessary every day to maintain dental health. Every other day or even a couple of times a week would suffice.
Sesame oil is most highly recommended for oil pulling. It is widely used in Ayurvedic medicine for massage, topical applications, etc. Typically, you would take one tablespoon (or one teaspoon for children) in the mouth, then sip, suck, and pull the oil through your teeth for 10 to 15 minutes, then spit out. The oil will turn milky white.
Sesame oil is naturally antibacterial, antifungal, and antiviral, which helps explain its ability to reduce S. mutans levels. If you don't have sesame oil, though, another oil that has many of the same properties and can also be used for oil pulling is coconut oil.


