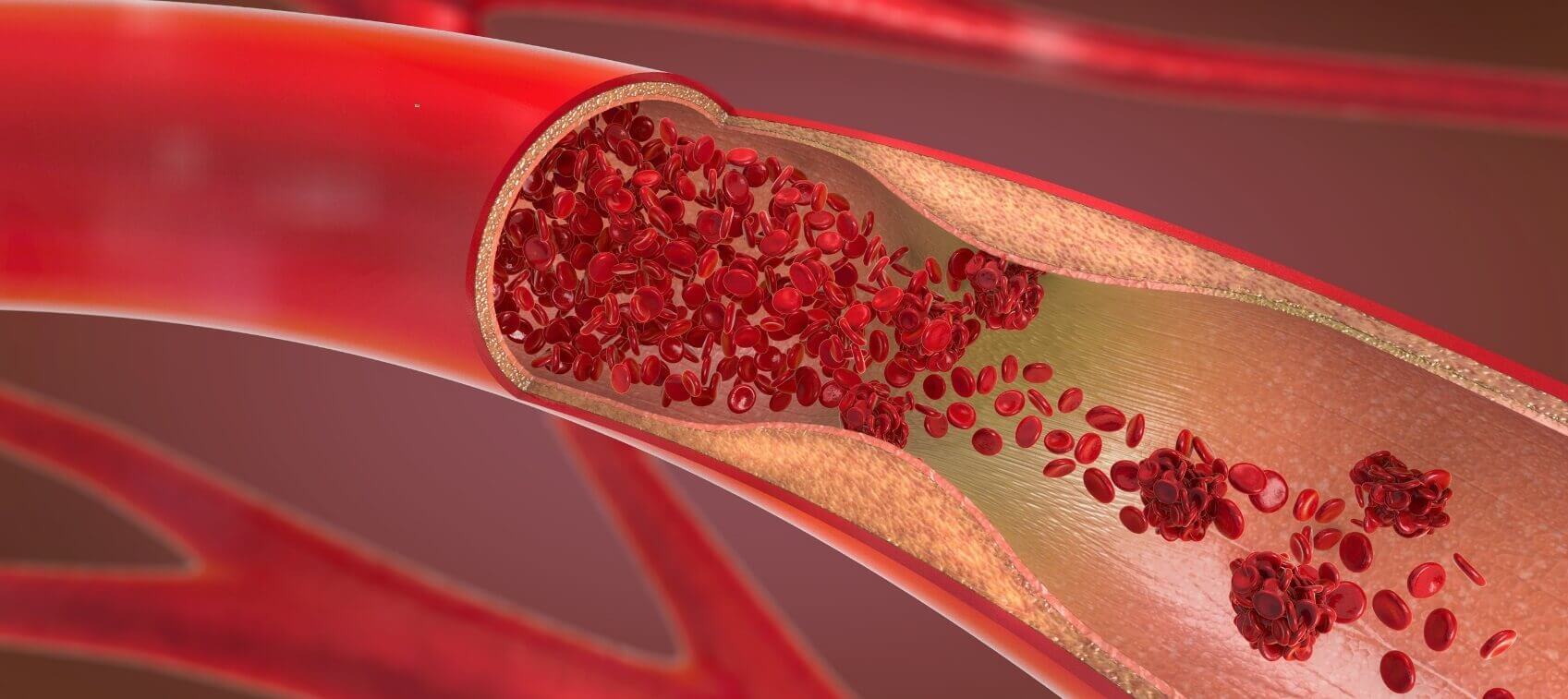
You may have heard of the term atherosclerosis, which refers to the buildup of plaque in the blood vessels. Essentially, coronary artery disease is a form of atherosclerosis that affects the arteries leading to the heart.
As plaque in the coronary arteries builds up and blockages grow, the level of oxygen and nutrients provided to the heart decreases, limiting the heart’s effectiveness. Should an artery become blocked completely—due to plaque buildup or the inability of a clot to pass through the narrowed opening—a heart attack results.
What Are the Symptoms of Coronary Artery Disease?
Since coronary arteries narrow slowly over time, it’s often difficult to diagnose in its early stages. One sign can include a rapid heartbeat during exercise or other exertion due to a heart that’s struggling from a lack of oxygen.
As narrowing of the coronary arteries progresses, symptoms can include:
- Angina
- Extreme fatigue or weakness
- Indigestion, heartburn or the feeling of needing to burp
- Pain radiating to the shoulders, neck, jaw/teeth, and arms
- Shortness of breath (which is an angina equivalent)
Inflammation can also signal that you are developing coronary artery disease. Markers of inflammation may include elevated levels of Lp(a), C-reactive protein (CRP), fibrinogen, homocysteine, interleukin 6, myeloperoxidase (MPO), and serum ferritin.
How to Test for Coronary Artery Disease
Evaluating the health of your coronary arteries is clearly key in determining your risk factors of heart disease, and avoiding a heart attack or stroke. Here are important tests to consider when assessing arterial health and heart disease risk.
Electron-Beam Computed Tomography (EBCT): This sophisticated, noninvasive screening measures calcium deposits in the coronary arteries. It’s proving to be a reliable way to assess heart attack risk factors in people with no (or few) other known risk factors. I strongly recommend EBCT as a screening tool for hidden, undiagnosed or silent heart disease. I consider any EBCT scan score over 100 to be a concern. Insurance may or may not pay for the scan.
64- or 128-Slice Coronary CT Scan: This test for detecting arterial plaque is even more advanced than EBCT. It’s the noninvasive equivalent of putting a camera inside the coronary arteries and assessing plaque and calcification status—with much less radiation than a coronary angiogram. If your cardiologist orders a standard, invasive angiogram for you, ask if a 64- or 128-slice coronary CT scan can be done instead.
Carotid Intima-Media Thickness Test (CIMT): This ultrasound imaging of the carotid artery measures the thickness of the inner layers of the carotid artery. Increased thickness is now considered a reliable, independent risk factor of heart disease and stroke. I highly recommend CIMT analysis because of its consistent ability to identify soft, transient plaque—and if you have soft plaque in the artery to the brain you are more likely to have soft plaque in the heart as well. So, CIMT is a safe and inexpensive method to help predict heart disease, as well as determine who really needs more invasive tests.
Coronary Angiogram: This procedure is considered the “gold standard” for evaluating the presence and extent of obstructive coronary heart disease. It’s performed while you’re awake after local anesthetic is injected into the groin area (to access the femoral artery) or the bend in the arm (if the brachial artery is used). Usually, we only use this test after a noninvasive procedure indicates the need. Angiograms are also used to evaluate heart valves, especially if surgery is being considered.
How to Prevent, and Reverse, Plaque Buildup in Arteries
Your diet is crucial for mitigating coronary artery disease. I strongly recommend an anti-inflammatory, low insulin-provoking (i.e. low carbohydrate) approach to eating—such as the Pan-Asian Modified Mediterranean (PAMM) diet.
Nutrients also play an important role. Here's my own current, complete daily regimen for plaque stabilization and reversal—which is the key to protecting yourself from coronary artery disease. I realize this list is long and comprehensive, so I have broken it down into two sections.
At a minimum, I highly recommend these six nutrients:
- A good, daily multivitamin/multimineral nutritional supplement
- Hydrosoluble CoQ10: 75-150 mg daily
- Magnesium: 400–800 mg daily
- Omega-3 Fatty Acids (squid or fish oil): 1-2 g daily
- Pomegranate Juice: 2–3 ounces daily
- Vitamin K2 Menaquinone-7 (MK-7): 150 mcg twice daily
Then, it is helpful to add:
- B-complex vitamins containing vitamin B12 (cobalamin), vitamin B6 (pyridoxine), folic acid, vitamin B1 (thiamin), riboflavin, and niacin, to mention a few
- Garlic (preferably the high allicin form): 1 g daily
- L-carnitine: 150–450 mg daily
- Vitamin C: 1 g daily
- Vitamin E: 200–300 units daily
Plus, you can also consider adding a daily cup of organic green tea to your diet.


